The healthcare industry is undergoing a rapid and substantial expansion, with projections indicating that the global healthcare budget will surge to an astounding $15 trillion USD by the year 2030. This surge signifies an escalating demand for adept healthcare administrators and managers possessing a visionary approach to address challenges, thereby propelling operations to new heights.
Remarkably, administrative costs constitute a significant portion, accounting for 34% of the total healthcare expenses in the United States. Within this dynamic landscape, healthcare administrators contend with a myriad of pressing issues daily, ranging from surging costs and regulatory shifts to operational bottlenecks, security imperatives, and the transformative impact of cutting-edge technologies.
For healthcare providers, the prospect of overlooking this rapid growth is not an option. To flourish in today’s swiftly evolving environment, they must embrace adaptability as a cornerstone. This blog is dedicated to illuminating healthcare’s prevalent administrative hurdles and providing insights and optimal strategies to confront some of the industry’s most paramount concerns.
Each team will face different concerns. Skip ahead by clicking a challenge below:
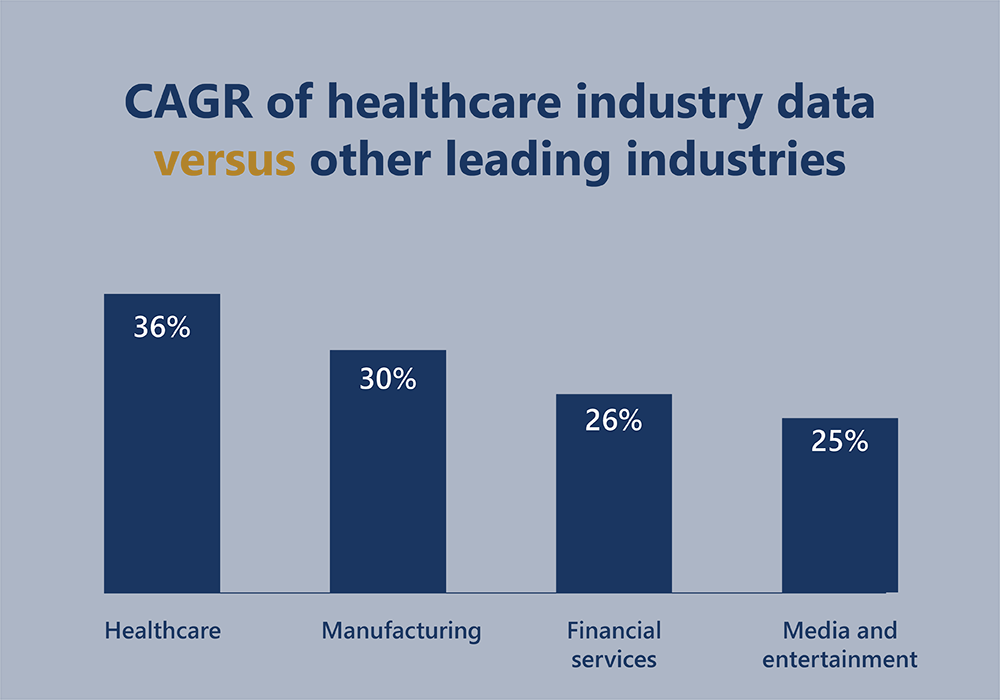
Effectively managing data is crucial in securing the future of healthcare. By 2025, it’s anticipated that a staggering 36% of the world’s data volume will stem from the healthcare sector, positioning it ahead of manufacturing, financial services, and media and entertainment. Refer to the accompanying image for a visual representation of this substantial growth in healthcare data compared to other industries.
Building a strategy to move forward
This surge in data necessitates a strategic approach from healthcare administrators. They must not only gather and interpret this data but also utilize it in meaningful ways to ensure the industry’s resilience. Given the diverse sources of data, administrators must prioritize best practices in data management, especially in financial contexts.
To navigate this data landscape effectively, investment in cloud-based solutions is imperative. These solutions offer comprehensive data visibility and advanced real-time reporting capabilities, enabling administrators to capitalize on this invaluable information. Too often, critical insights are lost in convoluted spreadsheets or outdated systems, which lack the agility required in an industry experiencing rapid expansion.
According to the American College of Healthcare Executives’ annual survey of issues confronting hospitals, financial challenges were the leading concern of hospital CEOs. Many point to the rising cost of healthcare due to the increase in insurance premiums and pharmaceuticals. However, financial concerns for the average clinic or hospital run much deeper than that.
The scope of concerns covers everything from consolidating financials across multiple health care units to managing medical billing, and denial and negotiating reimbursements. Robust financial management is vital. Most healthcare providers will require a digital transformation as the sheer scale of complexity would be impossible to handle manually. Our complete guide to financial management in healthcare is an online hub where we cover much of this information with videos, booklets and other resources.
Many are under pressure to expand and scale operations to serve the growing demand for services, which only adds to the complexity of their financial management. For instance, consolidating financial statements across multiple healthcare facilities is more involved than completing the period end report for one hospital.
For those with multiple healthcare units, check out our guides to financial consolidation:
As the demand for healthcare facilities surges, it’s no surprise that many healthcare providers will find themselves moving to new premises. Given the specialized nature of clinics and hospitals, finding a suitable space can be a costly venture. When your focus is on healthcare, the administration involved in managing and negotiating leases may come as an unwelcome complication.
Our blog on how to successfully negotiate medical facility leases sets out the best practices for healthcare providers looking to scale. It should give your administration team an idea of some of the challenges involved, such as tenant improvement allowances and exclusivity clauses.
Security is a growing concern of many healthcare providers. According to research, healthcare is particularly vulnerable to data breaches. Between February and May 2020, 132 breaches were reported in the US in large part due to the chaos introduced by COVID-19 that enabled scammers to take advantage while the industry struggled with a global crisis. It’s worth taking this risk and what it means for the future seriously, particularly given the amount of sensitive data stored by healthcare providers.
When it comes to protecting the financial health of your organization as you scale and grow, it’s worth investing in systems and solutions that boast advanced security options that protect you and your patient’s information. All accounting should take place in a highly secure environment that can store data and protect against threats.
Furthermore, it’s crucial to implement continuous monitoring and stay updated on the latest security protocols. As cyber threats evolve, so should our defences. Employing robust encryption technologies and implementing multi-factor authentication can provide additional layers of security for safeguarding sensitive information. By maintaining a proactive stance towards security, healthcare providers can fortify their defences against potential breaches and ensure the integrity of their data.
If you manage multiple healthcare units or are expanding, here are five steps to help you reduce and assess security risks.
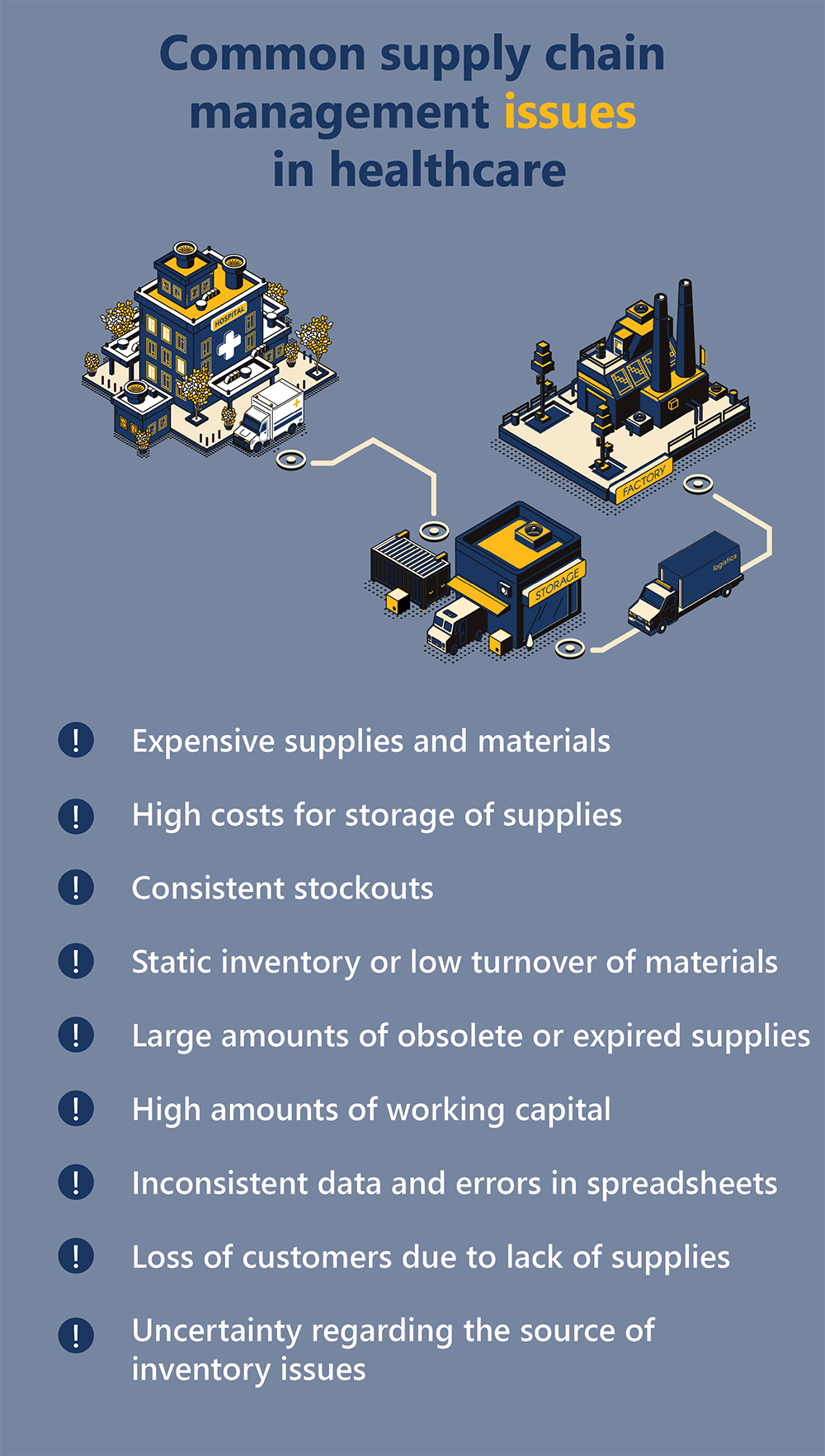
The supply chain is at the core of the healthcare industry, playing a pivotal role in its seamless operation. One of the most pressing challenges that administrators grapple with today revolves around the effective management of inventory.
This challenge is underscored by a range of common issues that frequently arise in healthcare supply chain management including expensive supplies and materials, high costs for storage of supplies, consistent stockouts, static inventory or low turnover of materials, large amounts of obsolete or expired supplies, high amounts of working capital, inconsistent data and errors in spreadsheets, loss of customers due to lack of supplies, and uncertainty regarding the source of inventory issues.
These challenges, while significant, are not insurmountable in today’s technologically advanced landscape. With the right software solutions in place, healthcare providers can address each of these issues effectively. Whether it’s optimizing inventory turnover or mitigating the costs associated with storage, modern technology offers practical solutions.
For those unsure about the urgency of supply chain management concerns in their facility, our guide to diagnosing and rectifying inventory issues provides a comprehensive resource. It aids in taking a step back, assessing any burgeoning inventory concerns, and addressing potential bottlenecks in the system. This proactive approach ensures that supply chain management remains robust and reliable, ultimately contributing to the seamless operation of healthcare facilities.
Remaining on top of changing healthcare regulations and policies is a critical facet of effective healthcare administration. The landscape of healthcare is continuously evolving, with new regulations and policies emerging to address the dynamic needs of the industry. Staying abreast of these changes is paramount for healthcare administrators to ensure that their organizations remain in compliance, provide quality care, and mitigate potential risks associated with non-compliance.
Adhering to global data management standards and regulations is another crucial aspect of maintaining a robust healthcare system. In addition to industry-specific standards like HIPAA in the United States, there are broader global data protection regulations that demand a high level of accountability in managing personal information. For instance, the General Data Protection Regulation (GDPR) in the European Union sets forth stringent requirements for the handling and protection of personal data. Healthcare providers operating on an international scale must navigate these complex regulatory frameworks to uphold patient privacy and data security.
By steadfastly abiding by these industry-specific and global standards, healthcare administrators not only ensure legal compliance but also instill trust in patients. This trust is a cornerstone of the patient-provider relationship, reinforcing the integrity of the healthcare system as a whole. It signifies a commitment to safeguarding patient information and prioritizing their well-being, which in turn, contributes to a culture of excellence and accountability within the healthcare organization.
Telemedicine and virtual healthcare have revolutionized the way healthcare is delivered, providing patients with the convenience of accessing medical services remotely. However, this shift has brought about a critical need for streamlined and automated complex billing solutions within the healthcare industry.
With the rise of telemedicine, healthcare providers are now catering to a larger patient base, many of whom prefer digital and automated methods for handling their bills. Patients expect fast, efficient, and hassle-free ways to make payments and receive invoices. Automating billing processes not only enhances the patient experience but also relieves the administrative team of the burden associated with manual billing tasks.
By implementing automated billing solutions, healthcare providers can significantly reduce the manual workload on their administrative teams. These solutions can handle tasks such as generating invoices, sending payment reminders, and processing payments. This allows the administrative team to focus on more critical tasks, such as consolidating financials and conducting thorough checks for errors or discrepancies.
One of the most significant advantages of automated billing in the context of telemedicine is its ability to provide immediate and accurate billing information to patients. This is particularly crucial for patients who need to make claims with their insurance providers promptly. With automated systems in place, patients can access their billing information in real-time, leading to faster and more efficient reimbursement processes.
For more information on modern billing, check out some of our key guides:
Revenue operations (RevOps) serves as a powerful framework and set of tools that can significantly enhance the management of every step along the patient journey in healthcare. This approach is particularly valuable for identifying friction points and aiding administrators in comprehending where bottlenecks and pain points may arise. Some of the areas RevOps can address include: resource allocation, workflow optimization, complex billing, patient pain points, end-to-end visibility, and friction resolution.
This is a relatively new concept for healthcare, and so we recommend checking out our guides to get a firm understanding of the power of this framework:
RevOps offers a tailored approach to healthcare, acknowledging its unique challenges and demands. By aligning sales, marketing, and customer success functions with revenue goals, healthcare providers can enhance patient satisfaction, operational efficiency, and financial viability. It is a fitting framework for healthcare and an essential one. It empowers healthcare providers to navigate the complexities of the patient journey, optimize workflows, and ultimately deliver higher-quality care. When implemented effectively, the approach can lead to a more patient-centric, efficient, and profitable healthcare operation.
In the realm of healthcare administration, recognizing the need for tailored, centralized solutions is paramount. Each healthcare facility operates with its own unique set of administrative challenges, from managing patient data to overseeing financial processes. A custom Enterprise Resource Planning (ERP) system designed specifically for healthcare can revolutionize operations by streamlining workflows, ensuring compliance, and enhancing overall efficiency.
To embark on this transformative journey, we encourage you to download our comprehensive custom ERP requirements checklist. This invaluable resource will serve as your blueprint, enabling you to meticulously outline the specific features and functionalities crucial to your healthcare facility.
By taking this proactive step, you’re poised to build a customized solution that perfectly aligns with your administrative needs, ultimately propelling your healthcare institution toward unprecedented levels of effectiveness and success. Don’t miss out on this opportunity to revolutionize your healthcare administration—download our checklist today and embark on the path to seamless, tailored operations.
Healthcare organizations are dependent on accurate and reliable information so they can provide the best possible care for their patients. At any given moment, there are typically hundreds of individual processes happening that all rely on accessing accurate data. However, the ever-growing amount and increasing complexity of data make it vital to invest in solutions to store and manage it efficiently.
Enterprise resource planning (ERP) software acts as the central nervous system within your organization. It gives you the power to manage and direct the different functions that need to occur to keep your organization healthy by integrating information from other departments into a centralized database.
ERP implementation in healthcare organizations modernizes your processes and operations, helps reduce costs, improve strategic and financial planning, and most importantly, enables you to provide better patient care.

Your organization can see an increase in productivity and a decrease in overhead when switching to an ERP system, as it creates a readily accessible, centralized database by integrating a wide range of operational requirements and departments (billing, inventory, supplies, finance, human resources, etc.).
For example, many facilities struggle with medical materials management resulting in expensive rush deliveries and shelves crowded with expired materials. Advanced supply chain management simplifies the process with automated replenishment from warehouses to sites while taking advantage of the best pricing available and collecting insights into all your vendor contracts.
Read more: 4 ways ERPs simplify financial consolidation for multi companies

Implementing an ERP can reduce expenses in a variety of ways, but they mainly cut costs by automating a range of operational processes. They can be programmed to precisely monitor finances and inventory levels, which reduces expensive administrative errors and optimizes operations at the back end like payroll, accounts, and inventory management.
Medical facilities with multiple entities need to perform intercompany transactions, consolidations, and mergers efficiently. The labour force and time required to finish these tasks manually can rack up a load of expenses. Look for centralized transaction processing to complete these transactions instantly with a lower rate of errors. That way, your staff can focus on the most important items without worrying about duplicated tasks or broken links.
The precise financial monitoring offered by ERPs not only helps keep track of cash inflows like patient payments, but also helps providers oversee their own expenditures. It can spot the needed and necessary improvements, offering key insights into budgeting, status of requisitions, and patient visitation analytics so decision makers can have a clearer understanding of the organization’s overall financial health.
It’s important that whichever software you choose provides real-time consolidated reporting because it allows your leaders to have the most up to date information at any given moment, increasing the agility of your organization and making it easier to overcome disruptions through quick pivots and future forecasts. Information is power and the depth of knowledge facilitated by ERPs lead to better financial planning, smarter business intelligence, and more accurate cost monitoring.
Read more: 6 essential financial consolidation software features for your company
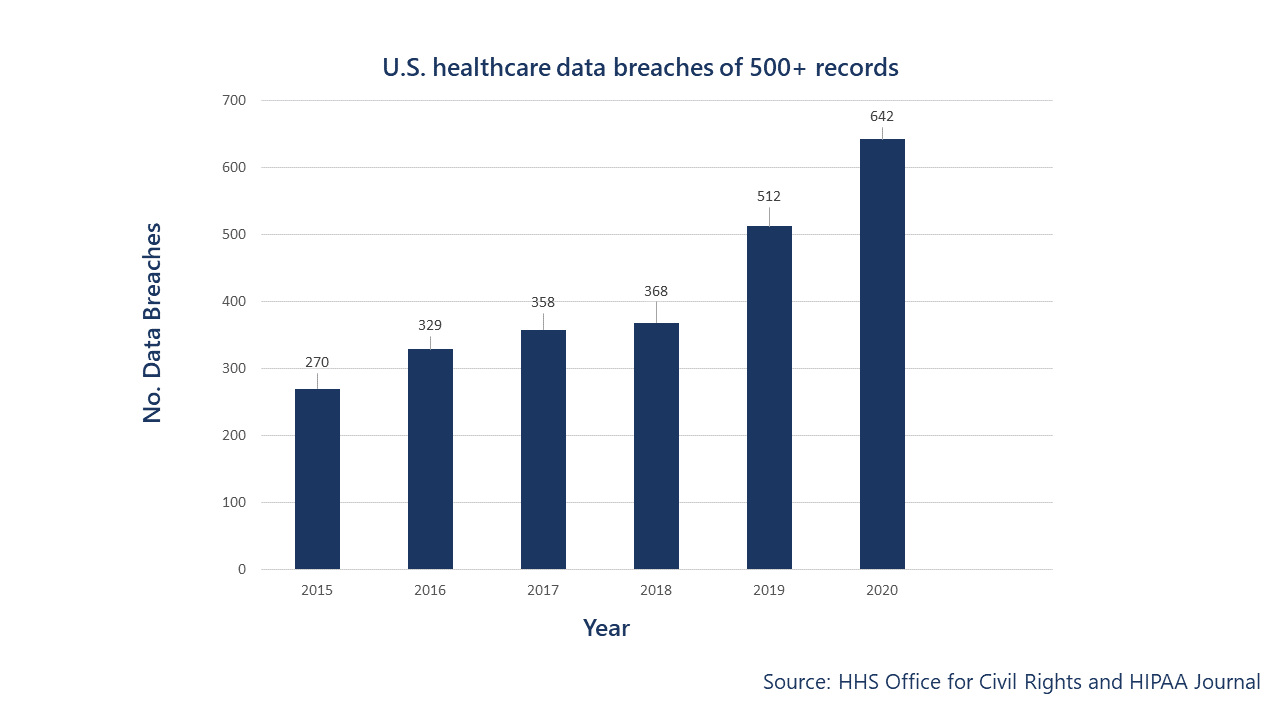
Medical records are confidential and involve sensitive information regarding the patient. Despite the high stakes associated with sensitive data, breaches still occur. In 2019, 32 million US patient records were exposed or otherwise impermissibly disclosed. In 2020, 1.76 data breaches of 500 or more healthcare records occurred each day.
The risk of a data breach increases when you’re transferring reports and sensitive information between multiple systems. When data is decentralized and managed via manual practices, strict maintenance of each system is required to prevent cyber threats. ERP software with a robust, scalable security system is more straightforward and will significantly reduce the risk of compromising your patients’ privacy.
One of the best parts is that it simplifies industry compliance. Failure to adhere to regulatory compliance can result in hefty fines and penalties. Violating HIPAA standards can cost anywhere from $100 to $1.5 million per year. It’s better to avoid the risk entirely by investing in infrastructure that facilitates compliance.
Paper-based and manual systems can make it difficult for nurses and medical staff to respond to a patient’s concern promptly, whether that’s booking their next appointment or discussing their billing plan. By switching to ERP software, a patient’s information can be stored in the master record and is accessible in one click. Easier access to financial records dramatically improves the patient experience.
ERP systems facilitate transparent communication between patients and medical staff and can retain that information across multiple facilities. The clarity of this data stream protects providers and patients alike in case an issue arises. Medical staff can also pair the software with patient portal services and manage the security settings to allow patients to see their records.
Bolstering your healthcare supply chain in an economic downturn may feel like a daunting task, particularly when the spread of COVID-19 accompanies that downturn. But it doesn’t have to be daunting. It’s possible to build long-term resilience into healthcare supply chains even during these uncertain times. Analysts predict that a recession is just around the corner, but the world is a very different place than it was for the last major economic crisis. This time around, it is possible to prepare by leveraging the intelligence of new technologies to weather the storm.
This recession will likely see an acceleration in the healthcare industry’s structural transformation. Strategic, adaptable healthcare facilities will survive, while those who remain mired in obsolete processes will struggle to survive. A situation that may be exacerbated by a rise in taxes as governments seek to plug the income gaps caused by shuttering companies.
It’s possible to not only survive an economic downturn but thrive in it. By investing time and money in developing agile healthcare supply chains, you should be able to bolster your organization against the worst of a recession. In this blog, we discuss how you should prepare.

Managing healthcare supply chains is a tricky job at the best of times—a well-managed supply chain is the backbone of any healthy organization. It ensures that all patients receive treatment in a timely fashion and saves lives. It also ensures that you keep both costs and inventories under tight control. A healthy supply chain is behind the smooth running of all day-to-day operations.
Because recessions generally mean uncertainty, those managing supply chains will have to rethink operations, and perhaps even technologies, to strategically address issues as they arise and increase efficiency. In unforgiving economic times, managing inventory will require you to assess your current supply chain and look for ways to improve at every level. The answer is not about small cosmetic changes but digging deep to bolster your organization and investing in processes and systems that reduce your team’s guesswork.
If you are already struggling with supply chain problems, you may be interested in reading our article on diagnosing and fixing supply chain issues. You can use this blog to help diagnose the existing issues you may be dealing with and perform a full audit of supply chain performance. A complete evaluation will be the first crucial step in this journey.
It can be easy to turn inward in times of uncertainty, but that would be a strategic mistake when optimizing your healthcare supply chain. Carefully monitor the financial health of your suppliers. Nobody is immune to the impact of a recession, and those suppliers who fail to commit to lean operations may find themselves in trouble during an economic downturn. As someone who relies on their product, you need to switch suppliers where necessary and have a list of back-up suppliers on hand. A thorough risk assessment will be essential to survival, so keep an eye on their financial health so that you do not suffer the disruption of suppliers’ losses.
One of the key parts of any supply chain is the supplier, and it’s likely that your suppliers will be negotiating with others at this time. Recessions lead to a drop in demand across the board, and so flexibility around pricing can occur that may not have been possible before the economic downturn.
Be sure to negotiate with suppliers and manufacturers to reduce costs and perhaps collaborate to ensure a constant supply of high-demand items while still reducing supply in other areas. You will have to be tactical and maximize supply while still minimizing the chance of stock-outs.
Your relationship with suppliers is not just about the next three months. Try to think ahead by at least three years and make tactical decisions based on the relationships you want to maintain and your organization’s overall costs.
Suppose you currently manage inventory within a basic ERP or spreadsheets. You may find it challenging to maintain a full perspective on your supply chain (particularly if you have multiple locations). To survive uncertain times, you will need to invest in digitizing supply chain management and having a centralized location that allows you to access your information in one place.
The ability to move quickly is vital in uncertain times and having clear insights can protect you by allowing you to make decisions immediately. It can often take weeks (or months) to consolidate the information you need to make significant decisions, but with the right software, it’s possible to access that information in hours.
Another benefit of investing in centralized ERP software for healthcare is the level of control it introduces. By automating processes, you reduce the number of errors in data and rest assured that the information you’re acting on is correct. You’re effectively creating a single source of truth and harnessing technology so that you can focus on strategically using the information at your fingertips to weather economic uncertainties.
Inventory management issues in healthcare supply chains are nothing new. For years, hospitals and long-term care facilities have seen expensive inventory go to waste, and unused materials tie up valuable storage space. Surplus stock, emergency “just-in-case” supplies, and shelf-life limitations all exacerbate these issues.
Supply chains have become something of a buzzword across most industries. When it comes to healthcare, the importance grows as materials are often needed to save lives. Introducing a systematic supply chain doesn’t just save time and money. It also frees up the minds of healthcare workers to worry about the patients, knowing that the materials they need will always be on hand.
But before you jump in, you must step back and diagnose the problems with your supply chain. It’s impossible to fix any issue without first fully understanding what’s causing it. In this blog, we will list the common inventory issues, then the steps to identifying your problems and creating a systematic supply chain that will never let your healthcare workers down.

No one person will be able to create this list. You must gather information from across your healthcare facility or facilities. A nurse may see different issues than the person in charge of storage, and the accounts team may be frustrated by something else entirely. Survey everyone involved at every link in the supply chain as you need a clear picture of all issues experienced.
You may find the list you end up with is quite long and covers a lot of ground. Try to break it up into categories that will help you better understand crossovers between issues. For instance, the inaccurate entry of data is likely to impact several areas of the supply chain.
If you’re unsure why a problem is happening, it is best to ask some questions. For example, if too many boxes of unused medications are taking up valuable storage space, it may be a good idea to follow the supply chain. You should figure out why exactly this is occurring.
It could be that orders occur on a recurring rotation without first checking existing supplies. It could also be a data entry issue or even just a member of the team with a desire to have extra supplies on hand. Once you know where the problem is coming from, it’s easier to prioritize this issue and decide how best to deal with it.
To prioritize the problems, you must identify which issues cause the most significant or most problematic losses. For example, you may find that incorrectly located material is a higher priority than overstocks because it impacts more lives. Equally, you may find that obsolete material is a priority as it ends up costing your healthcare facilities a lot of money.
Most supply chains will make financial justification the key to prioritizing a category, but when it comes to healthcare, the situation is more nuanced. Saving lives comes first, and so solving any issues that will result in better healthcare will most likely be a top priority.
You may not want to rush in with solutions just yet. Although you have a list of issues, you’ve no idea how frequently each one might occur. It’s best to start to track these occurrences so that you know which happens most often. If you have multiple locations, each team must track its inventory problems separately so that you can get a clearer idea of what is and isn’t working.
Set up a reporting system (a spreadsheet may work) that allows your team to record critical information about each issue. Essential information to record includes location, product, age of the stock, the issue with the stock, details as to why the problem occurred.
Before you start to solve the issues, you first need to tidy up the existing supply chain. Ensure all data is updated, expired items dealt with, and sort storage so that materials are in the right places. Once this short-term tidy is complete, you can begin to consider how best to fix the underlying issues.
Even with the best intentions, a short-term tidy up will only last so long. If the management of the supply chain does not change, it’s only a matter of time before the same inventory issues resurface.
A long-term solution will most likely include changes to the existing supply chain management processes and involving technology. Much of the issues in today’s healthcare supply chains come down to human error, obsolete processes, and poorly managed stock. By introducing automation to the supply chain, you will solve many of the issues.
Not only will a dedicated healthcare ERP solution solve data inconsistencies, but it can help you forecast the usage of stock, request material promptly, and enable users to scan and use items immediately. A system that automates the supply chain allows your team to get the job done quickly and efficiently without worrying about keeping track of materials after a long day treating patients. If you’re investing in an ERP, check out our blog on ten steps to help you build an ERP checklist.